Understanding Arterial Disease
Understanding Arterial Disease: Causes, Symptoms, and Treatment Options

Arterial disease is a condition that affects the blood vessels, specifically the arteries that carry oxygen-rich blood from your heart to the rest of your body. When these arteries become damaged or blocked, blood flow is restricted, which can lead to serious complications. Often underestimated, arterial disease is a common cause of heart attack, stroke, and even limb loss. Here’s a closer look at what arterial disease is, its causes and symptoms, and the treatment options that can help manage and prevent its progression.
What is Arterial Disease?
Arterial disease, often referred to as peripheral artery disease (PAD) when it affects the limbs, is typically caused by atherosclerosis—a buildup of fatty deposits, or plaque, inside the arteries. Over time, this plaque hardens and narrows the arteries, restricting blood flow and increasing the risk of clot formation. As a result, oxygen and nutrients struggle to reach vital organs and tissues, leading to symptoms that can range from mild discomfort to severe, life-threatening issues.
Causes of Arterial Disease
While some risk factors for arterial disease are unavoidable, others are linked to lifestyle choices and can be managed or reduced.
- Atherosclerosis: The most common cause of arterial disease, atherosclerosis occurs when cholesterol and fat accumulate in the arterial walls.
- Age: The risk of arterial disease increases with age, particularly for those over 50.
- Smoking: Smoking damages the blood vessels, increases plaque buildup, and significantly raises the risk of developing arterial disease.
- High Blood Pressure: Elevated blood pressure weakens the arteries over time, contributing to plaque formation.
- Diabetes: High blood sugar levels can damage blood vessels and accelerate plaque buildup.
- High Cholesterol: High levels of LDL (bad) cholesterol lead to plaque buildup, while low levels of HDL (good) cholesterol reduce the body’s ability to clear out plaque.
- Genetics: A family history of arterial disease can increase your risk.
Symptoms of Arterial Disease
Symptoms of arterial disease often go unnoticed until blood flow becomes severely restricted. When symptoms do appear, they may include:
- Pain or Cramping in the Legs: Known as claudication, this pain or discomfort in the legs (usually in the calves) occurs with walking or exercise and improves with rest. It’s often one of the first signs of PAD.
- Coldness in the Lower Leg or Foot: Restricted blood flow to the limbs can cause them to feel cold to the touch.
- Wounds That Don’t Heal: Reduced blood flow can slow down the body’s ability to heal cuts or sores, particularly on the feet.
- Skin Changes: Shiny or discolored skin, hair loss on the legs, or brittle toenails can all be signs of poor blood flow.
- Weak Pulse in the Legs or Feet: A reduced or absent pulse in the legs is often a sign of significant arterial disease.
- Erectile Dysfunction: In men, PAD can restrict blood flow, leading to erectile dysfunction.
When PAD becomes severe, patients may experience critical limb ischemia, which is marked by severe pain at rest, open sores, and the risk of gangrene. This condition requires immediate treatment to avoid complications.
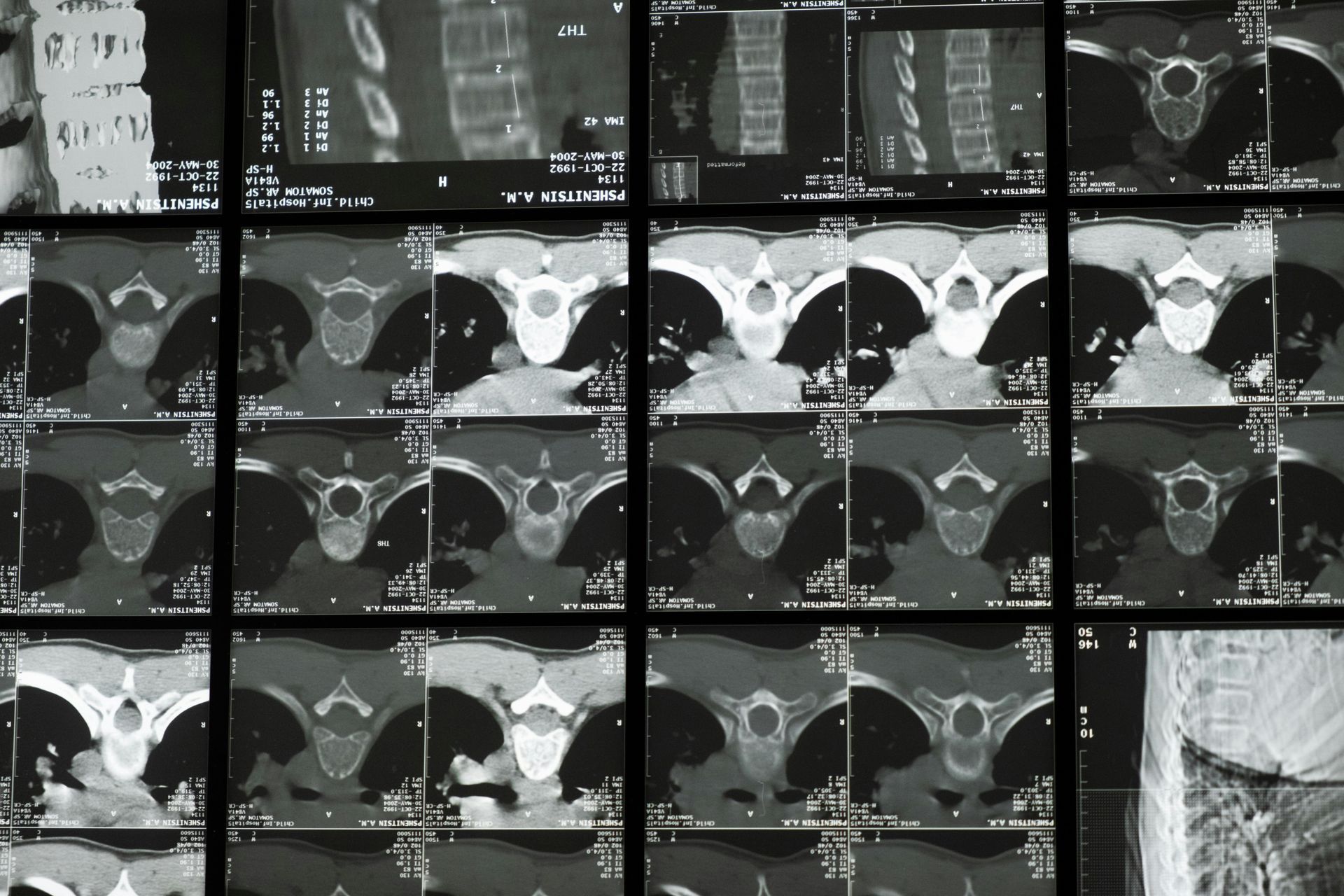
Diagnosing Arterial Disease
Detecting arterial disease early can be challenging, as symptoms often don’t appear until the disease is advanced. However, certain tests can help diagnose it:
- Ankle-Brachial Index (ABI): A non-invasive test that compares blood pressure in the ankle and arm to check for blockages.
- Ultrasound: This imaging test uses sound waves to measure blood flow in the arteries and detect blockages.
- Angiography: A more detailed imaging test where dye is injected into the arteries, allowing X-rays to detect narrowing or blockages.
- Blood Tests: Checking for high cholesterol and blood sugar levels can indicate an increased risk of arterial disease.
Treatment Options for Arterial Disease
Treatment for arterial disease focuses on slowing progression, managing symptoms, and improving quality of life. Options can include lifestyle changes, medications, and in more advanced cases, surgical intervention.
1. Lifestyle Changes
- Quitting Smoking: Stopping smoking is the most crucial step to slow the progression of arterial disease.
- Exercise: Regular, moderate exercise helps improve blood flow and can reduce symptoms of claudication.
- Healthy Diet: A heart-healthy diet, low in saturated fats, and high in fruits, vegetables, and whole grains can help control blood pressure, cholesterol, and blood sugar.
2. Medications
- Cholesterol-Lowering Drugs: Statins can help reduce cholesterol levels and slow down the progression of atherosclerosis.
- Blood Pressure Medications: Controlling blood pressure can help reduce strain on arteries.
- Blood Thinners: Medications like aspirin or clopidogrel can reduce the risk of blood clots.
- Diabetes Management: Controlling blood sugar levels is essential for slowing arterial disease in diabetic patients.
3. Interventional Procedures
For severe cases, interventional procedures or surgery may be needed:
- Angioplasty and Stenting: A catheter is used to open blocked arteries, and a stent is inserted to keep them open, improving blood flow.
- Atherectomy: This procedure involves removing plaque from the artery using a catheter with a cutting device.
- Bypass Surgery: In extreme cases, bypass surgery reroutes blood flow around a blocked artery using a graft.
Prevention: The Best Approach to Arterial Disease
The good news is that arterial disease can often be prevented or managed with a few healthy lifestyle changes. Regular check-ups, a balanced diet, staying active, and avoiding smoking are powerful steps that can protect your arteries and reduce your risk. If you notice any symptoms—like leg pain while walking or wounds that don’t heal—it’s essential to reach out to a healthcare provider sooner rather than later.
Arterial disease is a serious but manageable condition, and with early intervention, it’s possible to reduce symptoms, improve mobility, and enjoy a higher quality of life. If you’re at risk or experiencing symptoms, reaching out for assessment and care can help keep your arteries healthy and strong, supporting a vibrant, active life.